Upcoming newsletter does a review of protective underwear
Underestimated and Underfunded
Unlike breast cancer, whose advocacy campaigns have transformed awareness and funding, men’s health efforts remain diffuse and under-supported. This gap has slowed research, restricted outreach, and left many men untested until advanced stages.
10/21/20256 min read
The Unfunded Burden: Policy Inconsistency, Media Bias, and the Deficit in Advocacy for Prostate Cancer
Author: Anton João -Luiz Allensworth M.Ed.
Abstract
Prostate cancer remains the second-leading cause of cancer mortality among men in the United States, yet it continues to receive disproportionately low levels of research funding, advocacy, and public engagement compared to cancers with similar or lower mortality. This disparity reflects systemic failures in public health policy, funding priorities, and media representation rather than cultural stigma. This paper examines how inconsistent screening guidelines, episodic awareness campaigns, and gender bias in advocacy have constrained public understanding and limited early detection. It concludes with a set of policy recommendations addressing funding parity, screening guideline reform, and public–private collaboration to promote equitable outcomes and reduce preventable mortality among men.
1. Introduction
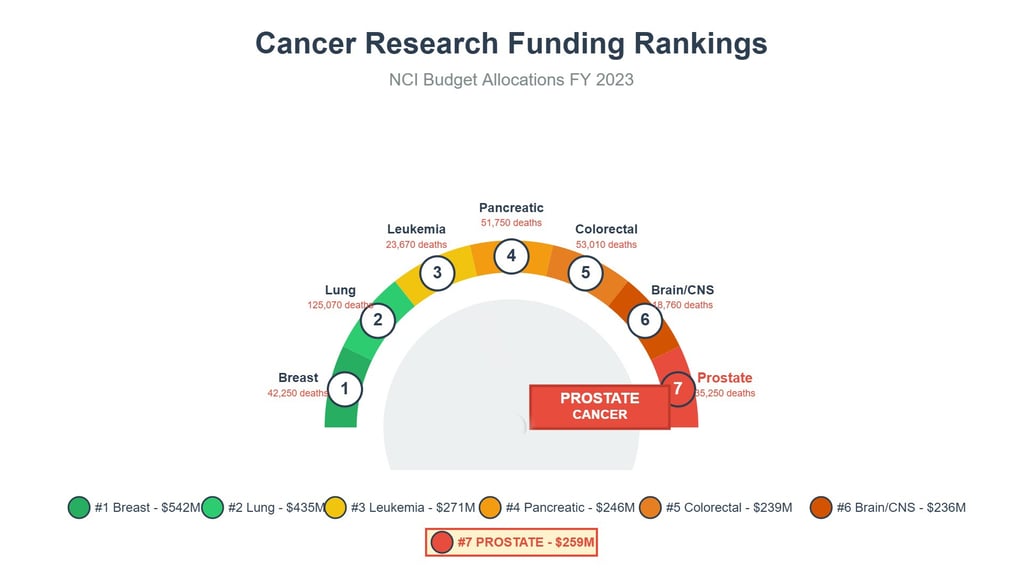
Prostate cancer remains one of the most significant public health challenges for men in the United States. With an estimated 313,780 new cases and 35,770 deaths projected for 2025, it continues to rank as the second-most lethal cancer among men.[1] Despite this burden, funding and advocacy remain markedly lower than for cancers with comparable incidence or mortality rates, such as breast cancer. This imbalance results in measurable losses—reduced survival outcomes, higher treatment costs, and diminished awareness among at-risk populations.
Contrary to cultural assumptions that men are reluctant to engage in preventive health behavior, the primary barriers are structural. They include inconsistent federal screening policies, the absence of continuous advocacy networks, and persistent gender bias in public health communication. Addressing these systemic deficiencies is essential to achieving parity in outcomes and ensuring men receive equitable attention in research, funding, and early detection efforts.
2. The Advocacy and Funding Disparity
Public health success often correlates with the degree of visibility, funding, and sustained advocacy a disease receives. When comparing prostate cancer with breast cancer, the discrepancy becomes stark. Over the past decade, breast cancer initiatives have secured billions more in federal funding and have maintained year-round visibility through coordinated campaigns. Prostate cancer, by contrast, relies primarily on short, event-driven initiatives such as annual awareness months.
Between 2013 and 2022, federal research investment in prostate cancer totaled approximately $3.6 billion, while breast cancer received more than $8 billion over the same period—a gap exceeding $4.5 billion.[2] The funding-to-incidence ratio for breast cancer was nearly double that of prostate cancer, indicating far more dollars spent per case. This disparity is not based on disease prevalence or severity but on the effectiveness of sustained advocacy networks and strategic communication.
Public engagement data reinforce this imbalance. Awareness metrics, including Google search volume and social media activity, show that breast cancer campaigns consistently generate several times more public interaction than those for prostate cancer. During their respective awareness months, breast cancer search activity increases by nearly 50%, while prostate cancer sees a modest 5% increase.[3] Social media engagement follows the same pattern, with breast cancer generating several hundred percent more activity each year. This attention imbalance has practical consequences: awareness drives policy, funding, and participation in early detection programs.
3. The Systemic Barrier: Conflicting Screening Policy
A consistent barrier to effective prostate cancer prevention has been conflicting guidance on prostate-specific antigen (PSA) screening. Rather than promoting unified clinical messaging, national policy has oscillated between discouragement and cautious endorsement, leaving both physicians and patients uncertain.
In 2012, the U.S. Preventive Services Task Force (USPSTF) issued a Grade D recommendation against routine PSA-based screening for all men, advising that the harms outweighed potential benefits. In 2018, the recommendation was revised to a Grade C for men aged 55 to 69, suggesting individualized decision-making after physician consultation, while still discouraging screening for men over 70.[4] These abrupt shifts have had measurable effects: PSA screening rates declined substantially after 2012, leading to an increase in late-stage diagnoses and poorer outcomes.[5]
This policy inconsistency has contributed to confusion among primary care providers and reduced public confidence in screening. When authoritative health agencies deliver contradictory guidance, the result is not informed choice but widespread uncertainty and disengagement. This uncertainty stands as one of the most significant, yet correctable, barriers to improving prostate cancer outcomes.
4. Economic and Societal Costs of Neglected Awareness
The failure to sustain consistent public messaging about prostate cancer carries measurable economic and societal costs. Lack of awareness leads directly to delayed diagnosis, forcing patients into costlier, more aggressive treatment pathways.
Research among Medicare beneficiaries demonstrates that the average cost of treating localized prostate cancer during the first year after diagnosis is roughly $7,600. In contrast, the cost of treating metastatic prostate cancer exceeds $58,000 during that same period—nearly eight times higher.[6] The transition from metastatic castration-sensitive to castration-resistant prostate cancer further triples monthly treatment expenses, imposing severe financial strain on both patients and healthcare systems.[7]
Beyond financial costs, there are psychological and productivity losses. Men diagnosed at later stages often experience higher rates of anxiety and depression, compounded by the physical side effects of treatment such as urinary and sexual dysfunction. Financial toxicity from prolonged therapy and loss of income further amplifies emotional distress. Collectively, these outcomes reduce productivity, erode quality of life, and strain national healthcare expenditures.
5. Policy Recommendations
The underfunding and fragmented advocacy for prostate cancer are not inevitable; they are policy-driven outcomes that can be corrected through deliberate action. The following recommendations outline a path toward sustainable parity in research, communication, and clinical practice.
5.1. Funding Parity and Federal Research Equity
Federal research funding should reflect the actual burden of disease, measured not only by incidence but also by mortality, morbidity, and economic cost. Congress and federal research agencies should adopt a parity-based funding formula to ensure prostate cancer receives resources proportional to its public health impact. A mortality-adjusted or disability-adjusted funding ratio would create a standardized benchmark, similar to those used in global burden of disease models.
To stimulate additional investment, public policy can incentivize private-sector giving through tax deductions or matching-grant programs for men’s health research. Encouraging corporate sponsorship, particularly from industries with large male consumer bases such as automotive, sports, and healthcare technology, can replicate the success achieved by breast cancer advocacy partnerships.
5.2. Screening Policy Reform and Clinical Communication
Reforming the USPSTF screening framework is central to rebuilding confidence in prostate cancer prevention. Policymakers should commission an independent review to harmonize PSA screening recommendations with the guidelines of professional societies such as the American Urological Association and the American Society of Clinical Oncology.
A unified national policy should encourage informed decision-making beginning at age 45 for average-risk men and at 40 for those with familial risk. Messaging must emphasize shared decision-making between physicians and patients rather than passive avoidance of screening. Once a clear standard is established, agencies like the Centers for Disease Control and Prevention can lead a consistent national education campaign to restore public trust and clinician confidence.
5.3. Sustained Advocacy Through Public–Private Partnerships
The success of awareness campaigns depends on persistent communication, not annual observances. Policymakers and nonprofit leaders should collaborate to establish a year-round advocacy infrastructure for prostate cancer. This can be achieved by forming coalitions that include government agencies, employers, community organizations, and healthcare providers.
Co-branded campaigns similar to those used in women’s health—featuring recognizable visual identities, corporate participation, and consistent messaging—should be developed to normalize prostate cancer testing and encourage early detection. Public–private partnerships can expand outreach into workplaces, sports organizations, and community health centers, ensuring the message reaches men in diverse social and economic settings.
5.4. Data Collection and Accountability
Federal and state health agencies should track prostate cancer awareness and funding metrics annually to ensure sustained progress. Data transparency will allow for public accountability and facilitate adaptive policymaking. Regular reporting of screening rates, research investment levels, and mortality trends will help policymakers evaluate the success of reforms and maintain a focus on continuous improvement.
6. Conclusion
Prostate cancer’s enduring position as the second-leading cause of cancer death among men reflects a preventable policy failure, not a biological inevitability. The evidence is clear: early detection saves lives, yet inconsistent screening policies, fragmented advocacy, and insufficient funding have perpetuated indifference and confusion.
To reverse this trend, policymakers, clinicians, and advocacy organizations must commit to a unified, sustained strategy. Funding parity with comparable diseases, consistent national screening guidance, and collaborative advocacy partnerships represent not merely symbolic reforms but actionable measures that can save thousands of lives each year.
Equitable attention to prostate cancer is both a clinical imperative and a moral responsibility—an essential step toward ensuring that men receive the same commitment to awareness, research, and compassion that other populations have long benefited from.
Endnotes
SEER. (2025). Cancer Stat Facts: Common cancer sites (2025 estimates).
ASCO. (2023). Disparities in NIH and federal cancer research funding across different cancer types.
Anticancer Research. (2023). Following the trend: A comparative analysis of public engagement and funding for annual prostate and breast cancer campaigns using Google Trends.
United States Preventive Services Task Force. (2018). Recommendation: Prostate cancer screening.
American Cancer Society. (2024). Cancer statistics, 2024.
Tandfonline. (2022). Cost of cancer management by stage at diagnosis among Medicare beneficiaries.
Journal of Managed Care Pharmacy. (2024). Real-world economic burden associated with disease progression from metastatic castration-sensitive to castration-resistant prostate cancer on treatment in the United States.
info@crownsproject.org
1 (330) 554-0099
Subscribe for NEWSLETTER updates
© Copyright 2026 The Crowns Project. All rights reserved. The Crowns Project is a national 501 (c)(3) organization dedicated to providing educational resources, access, and assistance to aid in the early detection, treatment, and survival of prostate cancer
general inforomation